When purchasing health insurance, making an informed decision is important to ensure the proper coverage. Below are a few things to consider before making your choice:
1. Waiting Period
A waiting period is the time you need to wait before you can make a claim for some or all benefits of your health insurance policy.
This waiting period and its terms and conditions will vary from company to company. Usually, there is an initial waiting period of around 30 days after which you can actively start using your health insurance (except for accidental hospitalization). There are also specific waiting periods for pre-existing diseases, maternity benefits, and for certain other ailments.
2. Co-payment
A co-payment refers to the percentage of the claim amount that will be borne by the policyholder during a claim in health insurance. Essentially, it means you and your insurer will be splitting the medical bills; so, while your insurer will pay for a large portion of the bill, a smaller part of it would have to be paid by you. For example, if you have a 15% co-pay, your insurer will bear 85% of the claim amount, while you pay the rest.
While opting for a higher co-pay, it will help to lower your total premium, it will mean that you have to pay a larger amount during claims. On the other hand, a lower co-pay will increase your premium, but in the end, you will pay less during claims.
Some insurance policies come with a mandatory clause for co-payment, while others will offer policyholders the option to choose a voluntary co-payment amount.
3. Cashless Health Insurance
Instead of getting your hospital bills reimbursed from your health insurer after your treatments, a cashless health insurance is where after you get the required treatment at a Network Hospital, your health insurer will take care of the bills directly. You don’t need to pay any cash out of your own pocket.
All you need is an approval from your insurer or third-party administrator, and the costs will be taken care of between the hospital and your insurance company.
4. Pre and Post Hospitalization
Medical bills often go beyond what you need to pay for your hospitalization stay.
Pre-hospitalization expenses are those that are incurred before you are admitted to the hospital for treatment, such as diagnostic tests, investigative procedures, medication, and more.
Post-hospitalization expenses refer to the medical costs incurred between 45-90 days after you are discharged from the hospital after your treatment. This could include follow-up tests, continuing treatments, specific medications, etc.
5. Room Rent Capping
When you are hospitalized, the hospital will charge you a room rent for the time that you are admitted. There are a range of hospital rooms like a general ward, double room, deluxe room, luxury room, etc. with a different room rent of each.
Many insurance providers set a maximum room rent limit under their health insurance, including a cap on ICU room rents as well. So, in case you choose a hospital room with a higher rent, you would have to pay the extra amount out of your pocket. For example, if your rent charges are capped at 1% of your sum insured of ₹5 lakhs, your insurance will cover the same up to ₹5,000.
However, some insurance companies like Digit have no room rent capping as a benefit, meaning that you can choose any hospital room you want during your treatment as long as your total claim amount doesn’t exceed your sum insured.
6. Pre-existing Diseases
Pre-existing diseases or conditions are any disease or health condition that you already have had symptoms of or have been treated for within 36 months before you got your health insurance policy. These can range from serious conditions like cancer or diabetes to high blood pressure, or asthma.
Depending on your age and the disease or condition, there is usually a 3 year waiting period before a pre-existing condition is covered.
When it comes to pre-existing diseases, it’s best to be as transparent as possible! Include all the diseases and treatments you would need covered in your health insurance policy so that your insurance provider won’t reject your claims later.
7. New Age Treatments
With the success of technological improvements in modern medicine, a number of “new-age” procedures are also sometimes covered as a part of your health insurance policy. They include treatments like:
- Balloon sinuplasty
- Deep brain stimulation
- Oral chemotherapy
- Immunotherapy
- Uterine Artery Embolization and HIFU (High intensity focused ultrasound)
- Intra vitreal injections
- Robotic surgeries
- Stereotactic radio surgeries
- Bronchial thermoplasty
- Vaporization of the prostate
- IONM (Intra Operative Neuro Monitoring)
- Stem cell therapy
Often these procedures are covered up to 50% of the total sum insured.
8. Daycare Procedures
Daycare treatments and procedures are those medical treatments that need hospitalization, but for less than 24-hours. So, it is when you need to be admitted to the hospital for a treatment or operation that takes less than a day.
Some examples of daycare treatments include cataract surgeries, nasal sinus aspiration, cancer chemotherapy, cancer radiotherapy, etc.
9. Add-on Covers
On the other hand, additional covers (also called add-ons or riders) are additional coverages that you can opt for in addition to your existing health insurance policy. When you have these covers you can enhance your coverage for an additional premium.
According to the IRDAI, the total premium for all the add-ons picked under a single health insurance policy cannot exceed 30% of the original premium amount. So, if you get a family floater health insurance at ₹5,000/year, and you want to include 5 add-ons, the additional premium you will need to pay for those add-ons cannot exceed ₹15,00 (30% of 5000).
Popular add-ons include features like a Maternity cover, Room Rent waiver, Hospital cash cover, or critical illness cover.
10. Exclusions
Often, there are limits and restrictions to your health insurance policy, such as diseases, conditions or situations where your medical expenses will not be covered. There are two main types of exclusions:
- Permanent Exclusions – these are never covered by your policy, and can include things like hospitalization without a doctor’s recommendation, or pre-natal and post-natal medical expenses.
- First Year Exclusions – these are specific diseases or treatments that are only covered from the second year of your policy, such as those with longer waiting periods like cataracts, hernia, endometriosis, or neurodegenerative disorders.
It is important to know what is excluded in your policy before you purchase it so that there are no surprises when it is time to make a claim.
11. Sum Insured
Your sum insured is the maximum amount your health insurer will be able to cover for you in one year in case of medical claims. Thus, it is the maximum reimbursement you can get in case you make a claim with your health insurer.
In case your total medical bills exceed this amount, you will have to pay the extra cost out of your own pocket. Thus it is important to choose the SI carefully.
While a lower SI can result in a lower premium, when you opt for a higher sum insured, you will be increasing the amount you have in case of emergency
12. Cumulative Bonus
A cumulative bonus is similar to a no claim bonus in car insurance. However, instead of an upfront discount, you will get added benefits.
In case you haven’t made any claims during the policy year, will give you an increase in your Sum Insured, without charging you any extra premium. This increase in your sum insured is called a cumulative bonus. It usually starts at 10% for every claim-free year.
13. Deductible
Some health insurance plans include a deductible. This is when you need to pay a part of the insurance claim from your pocket before the insurer can cover the rest for you. This amount is usually decided by you while buying your health insurance policy.
So, for example, if your healthcare claim is ₹35,000, and you have a deductible amount of ₹10,000, your insurance company will be liable to pay ₹25,000. The ₹10,000 deductibles will have to be borne by you.
There are two types of deductibles – Compulsory and Voluntary.




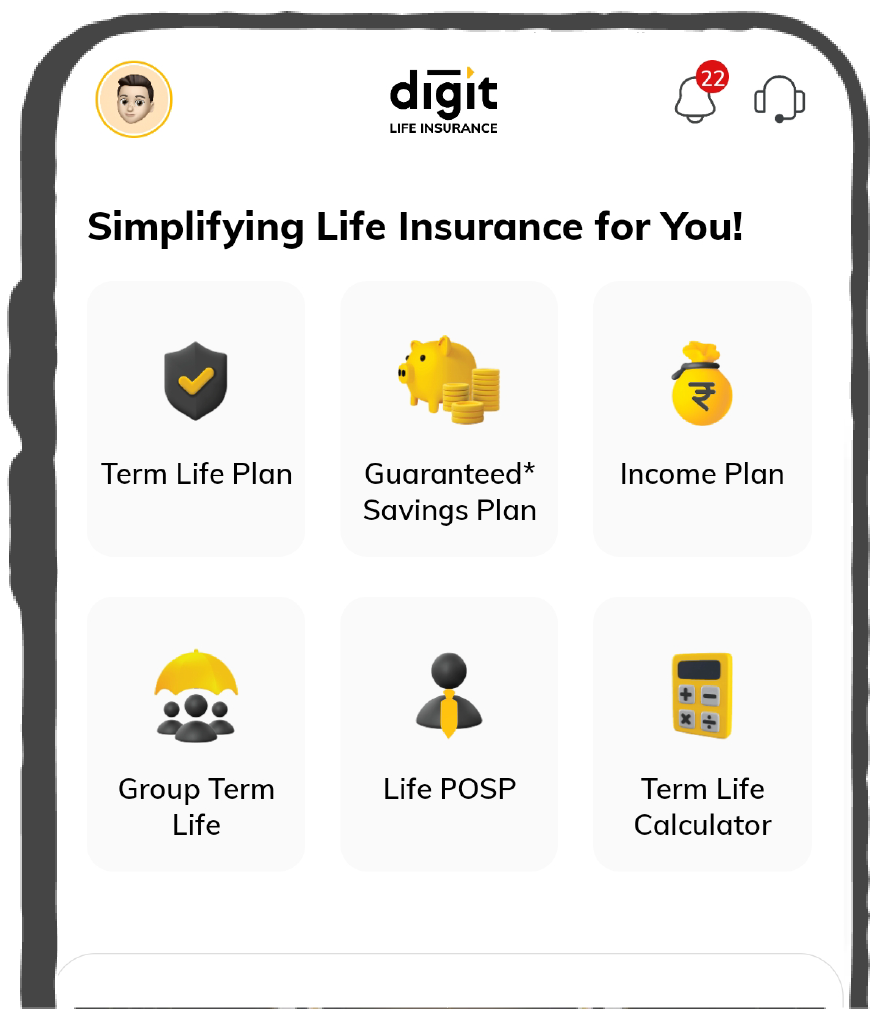






 Tools & Calculators
Tools & Calculators