×

General
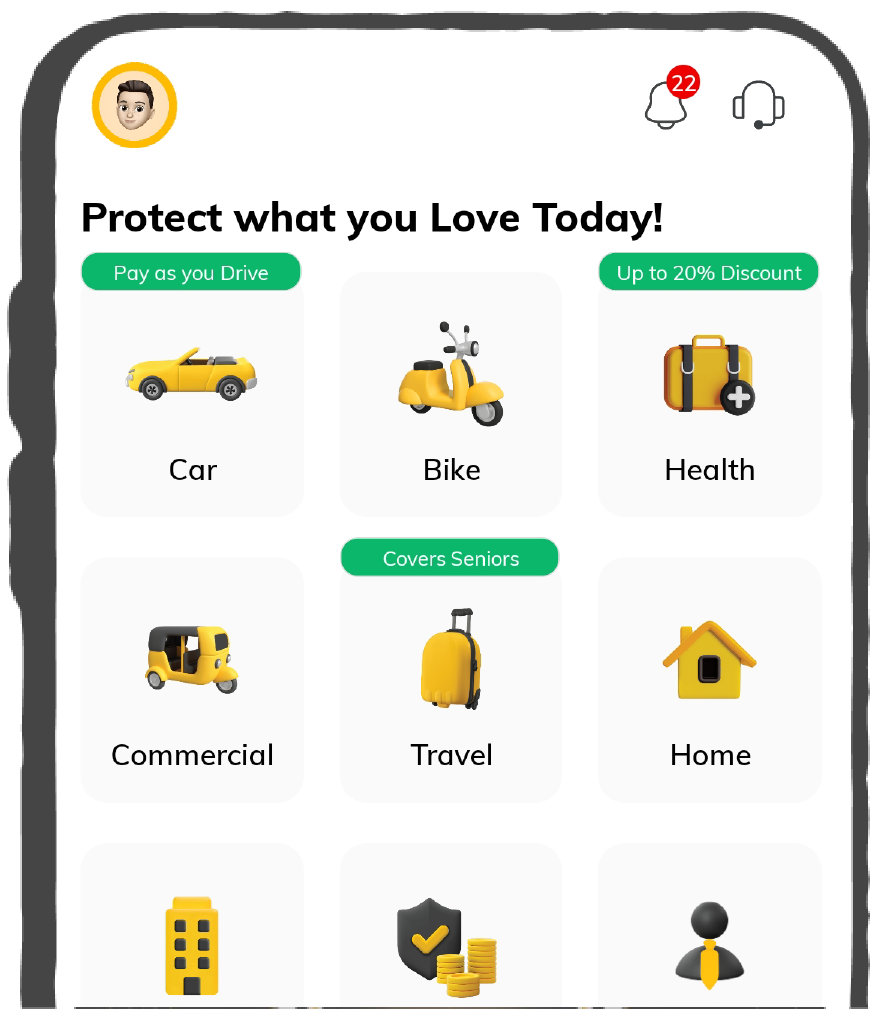
General Products
Simple & Transparent! Policies that match all your insurance needs.
General Insurance


Rated App
37K+ Reviews
Rated App
7K+ Reviews
Scan to download
Life
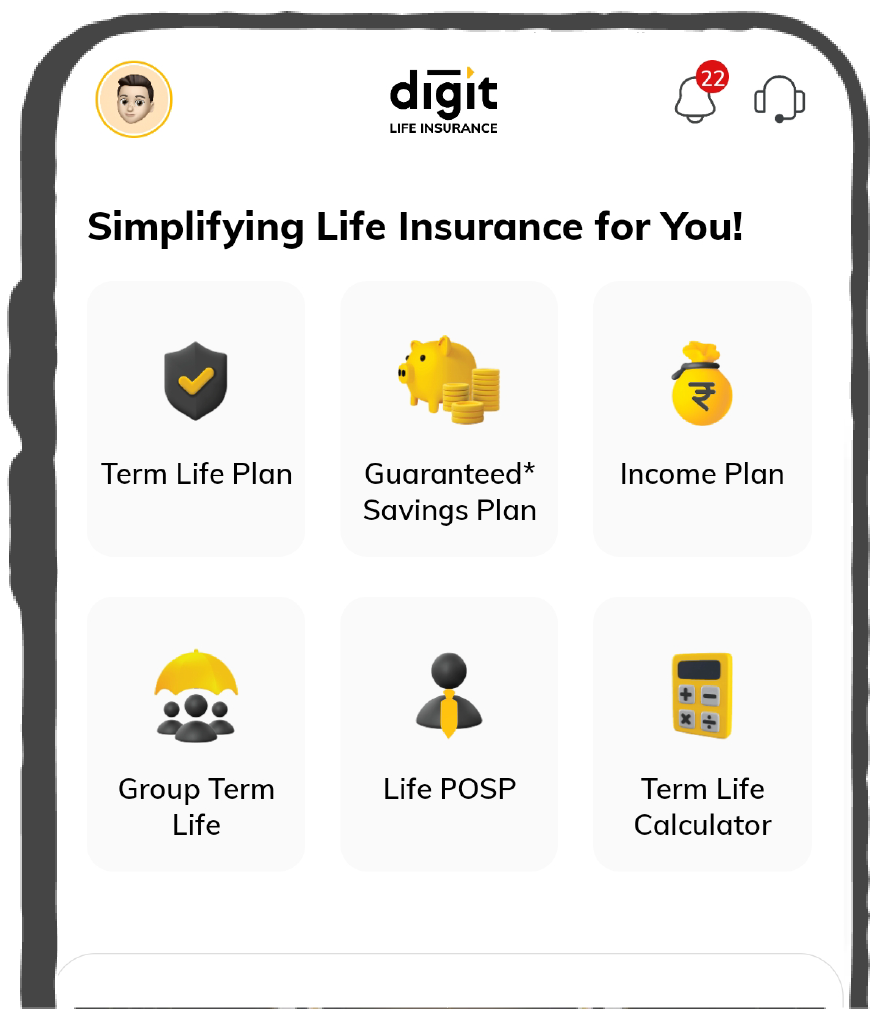
Life Products
Digit Life is here! To help you save & secure your loved ones' future in the most simplified way.
Life Insurance


Rated App
37K+ Reviews
Rated App
7K+ Reviews
Scan to download
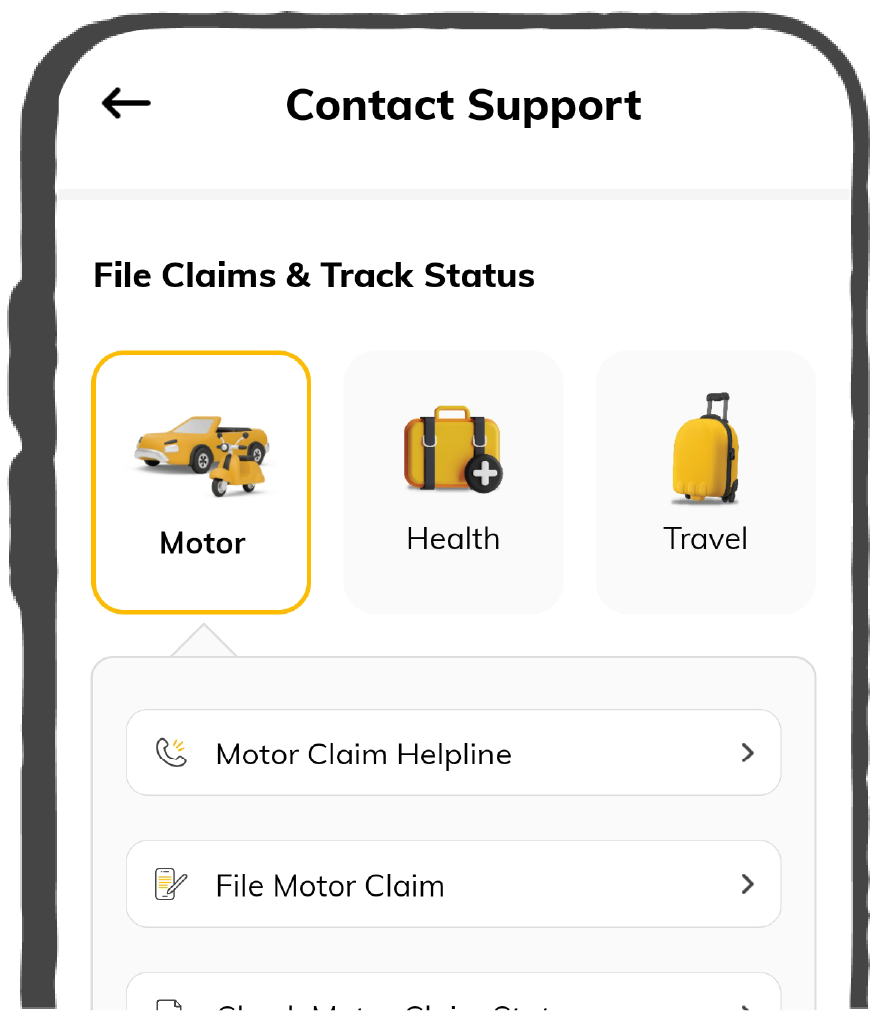
Claims
Claims
We'll be there! Whenever and however you'll need us.
Claims


Rated App
37K+ Reviews
Rated App
7K+ Reviews
Scan to download
Renewals

Renewals
General
Become an Agent

Resources
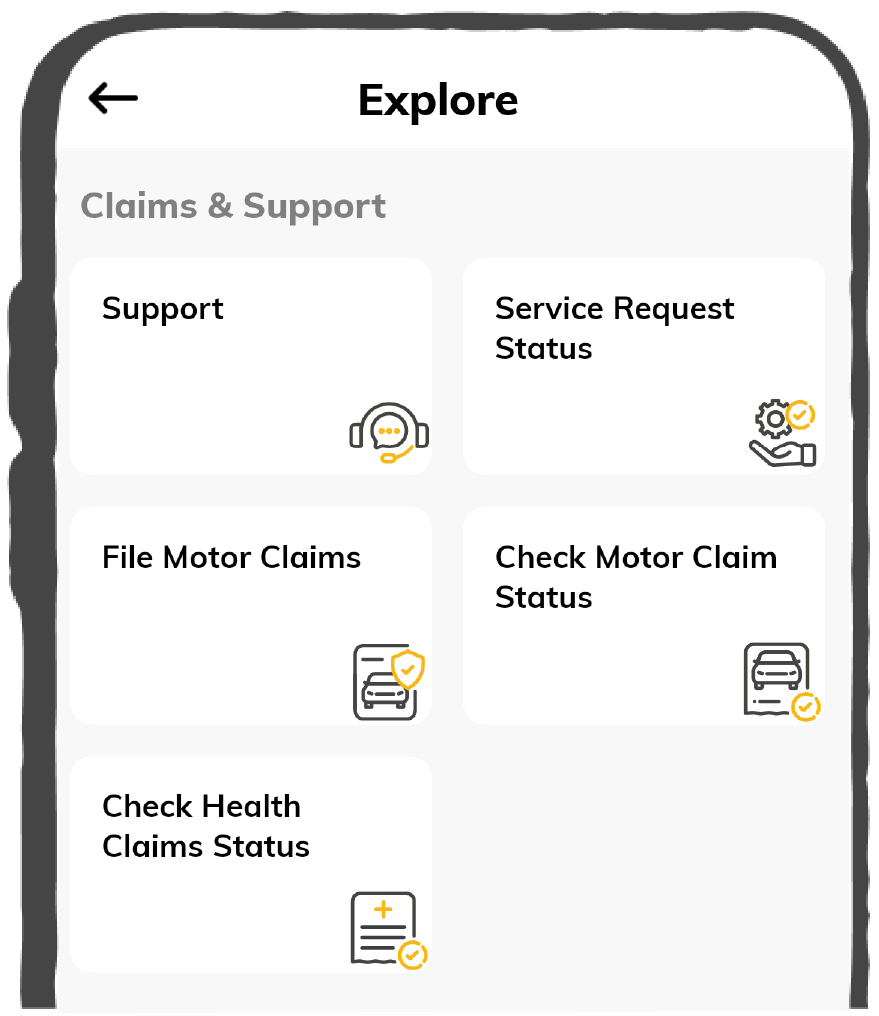
Resources
All the more reasons to feel the Digit simplicity in your life!
Resources

 Tools & Calculators
Tools & Calculators

Rated App
37K+ Reviews
Rated App
7K+ Reviews
Scan to download
Rated App
37K+ Reviews
Rated App
7K+ Reviews
Our WhatsApp number cannot be used for calls. This is a chat only number.

Powered By Digit












