Cashless Health Insurance
Buy Cashless Health Insurance Online
9000+
Cashless Hospitals
2.5 Crore+
Lives Insured
4.5 Lacs+
Claims Settled
I agree to the Terms & Conditions
Get Exclusive Porting Benefits

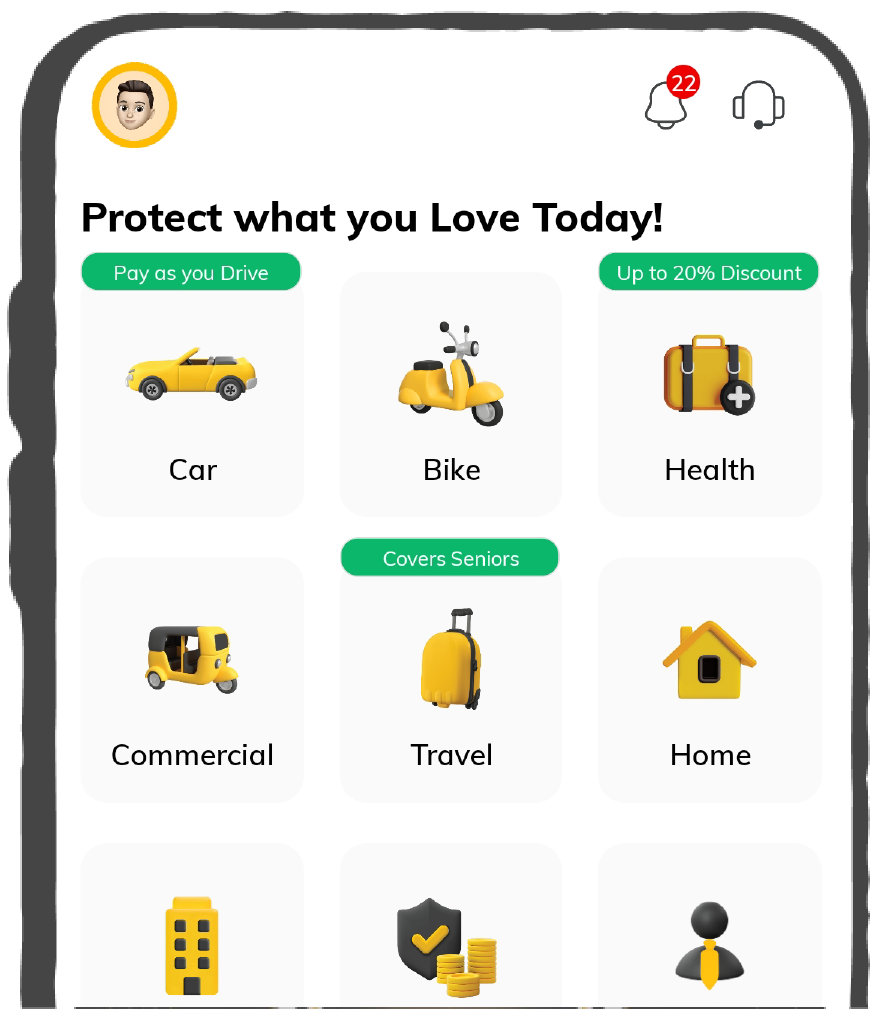
Buy Health Insurance, Up to 20% Discount
Port Existing Policy
9000+
Cashless Hospitals
2.5 Crore+
Lives Insured
4.5 Lacs+
Claims Settled
What is a Cashless Health Insurance Plan?
Cashless health insurance refers to a health insurance plans that gives you the choice to opt for your required treatment, without having to pay any cash out of your own pocket. The same costs are directly taken care of by the hospital and your health insurer (us!).
For example: If you or a family member is affected with the coronavirus and needs to be admitted for treatment, a cashless medical insurance will ensure you don’t need to pay upfront for the costs of the same.
All you need is an approval from your health insurer or third-party administrator and the rest will be taken care of by your health insurer!
What is a Cashless Claim?
Imagine being admitted to a hospital because of an illness and you have to pay nothing! Unbelievable, Right? But yes, this is possible because of Cashless Claims.
In a cashless claim, the hospital and your insurance company/TPA will work together to arrange and pay the bill according to your policy's coverage, but only if you undergo the treatment in an affiliated hospital.
How Does Cashless Claim Work?
A cashless claim is a simple process. Cashless health insurance ensures cashless treatment anywhere, removing the inconvenience of paying cash at hospitals when necessary:
- Choose Your Insurance Company: You start by selecting a health insurance provider that meets your requirements.
- Select Your Plan: Based on your needs and financial situation, you choose a health insurance plan with cashless benefits.
- Purchase the Plan: Pay the premium and purchase the policy to get the benefit in emergencies.
- Locate a Network Hospital: Look for a network hospital that has partnered with your insurance company for treatment.
- Use Your Health E-Card: When you visit a network hospital, you must download your health E-Card containing all your information and show it to the hospital.
- Your Insurance Pays the Bill: Depending on your policy, the hospital and insurer will cover the cost of the treatment.
Why is Cashless Health Insurance Important?
Who doesn't like to be stress-free while undergoing treatment? A cashless medical insurance policy is important to protect you from hefty medical bills. Here are some other important things about having cashless health insurance.
Why Choose Cashless Health Insurance by Digit?
What’s Covered in the Health Insurance Plans Offered by Digit?
Coverages
Double Wallet Plan
Infinity Wallet Plan
Worldwide Treatment Plan
Important Features
This covers for all hospitalisation expenses including due to an Illness, Accident, Critical Illness or even pandemics like Covid 19. It can be used to cover for multiple hospitalisations, as long as the total expenses are up to your sum insured.
You need to wait for a defined period from the first day of your policy to get covered for treatment related to any non-accidental illness. This is the Initial Waiting period.
Exclusive Wellness Benefits like Home Healthcare, Tele consultations, Yoga and Mindfullness and many more available on our App.
We provide a back-up Sum Insured which is 100% of your Sum Insured amount. How does Sum Insured Back Up work? Suppose your policy Sum Insured is Rs. 5 lac. You make a claim of Rs.50,000. Digit automatically triggers the wallet benefit. So you now have 4.5lac + 5 lac Sum Insured available for the year. However, one single claim, cannot be more than the base Sum Insured as in the above case, 5 lac. .
 Digit Special
Digit Special
No claims in the Policy year? You get a bonus -an additional amount in your total sum-insured for staying healthy & claim free!
Different categories of rooms have different rents. Just like how hotel rooms have tarrifs. Digit plans give you the benefit of having no room rent cap, as long as it is below your Sum Insured..
Health insurance covers medical expenses only for hospitalisations exceeding 24 hours. Day care procedures refer to medical treatments undertaken in a hospital, requiring less than 24 hours due to technological advancement such as cataract, dialysis etc.
 Digit Special
Digit Special
Get a world class treatment with the Worldwide Coverage! If your doctor identifies an illness during your health examination in India and you wish to get a treatment abroad, then we’re there for you.You’re covered!
We pay for your health check-up expenses upto the amount mentioned in your Plan. No restrictions on the kind of tests! Be it ECG or Thyroid Profile. Make sure you go through your policy schedule to check the claim limit.
There may be emergency life-threatening health conditions which may require immediate transportation to hospital. We absolutely understand this and reimburse for expenses incurred for your transportation to a hospital in airplane or helicopter.
 Digit Special
Digit Special
Co-Payment means a cost sharing requirement under a Health Insurance Policy that provides that the Policyholder/Insured will bear a specified percentage of the admissible claims amount. It does not reduce the Sum Insured. This percentage depends on various factors like age, or sometimes also on your treatment city called zone based copayment. In our plans, there is no age based or zone based Co payment involved.
Get reimbursed for the expenses of road ambulance, in case you are hospitalised.
This cover is for all expenses before and after hospitalisation such as for diagnosis, tests and recovery.
Other Features
The disease or condition that you are already suffering with and have disclosed to us before taking the policy and has been accepted by us has a waiting period as per plan opted and mentioned in your Policy Schedule.
This is the amount of time you need to wait for, until you can make a claim for a specific illness. At Digit it is 1-3 years and starts from the day of policy activation. For the full list of exclusions, read Standard Exclusions (Excl02) of your policy wordings.
If You sustain an Accidental Bodily Injury during the Policy Period, which is the sole and direct cause of Your Death within twelve (12) months from the date of accident, then We will pay 100% of the Sum Insured as mentioned in Policy Schedule against this cover and as per plan opted.
 Digit Special
Digit Special
Your organ donor gets covered in your policy. We also take care the pre and post hospitalisation expenses of the donor. Organ donating is one of the kindest deeds ever and we thought to ourselves, why not be a part of it!
Hospitals can go out of beds, or the patient’s condition may be rough to get admitted in a hospital. Don’t panic! We cover you for the medical expenses even if you get treatment at home.
Obesity may be the root cause of so many health issues. We absolutely understand this, and cover for Bariatric Surgery when it is medically necessary and advised by your doctor. However, we DONOT cover if hospitalisation for this treatment is for cosmetic reasons.
If due to a trauma, a member has to be hospitalised for a psychiatric treatment, it will be covered under this benefit, upto INR 1,00,000. However, OPD consultations are not covered under this. The waiting period for Psychiatric Illness Cover is same as Specific Illness waiting period.
Before, during & after hospitalisation, there are many other medical aids & expenditures such as walking aids, crepe bandages, belts, etc.,which need your pocket’s attention.This cover takes care of these expenses that are otherwise excluded from the policy.
What’s Not Covered?
Add-on Options for Cashless Health Insurance with Digit
Enhance your cashless health insurance policy with add-ons at Digit. These add-ons are subject to underwriting approval and your eligibility at the time of purchase or renewal. Here’s a list of add-ons available that provide additional layers of protection beyond the basic coverage of your policy:
Key Benefits of Cashless Health Insurance by Digit
Your health insurance plan with Digit extends several exclusive benefits that enhance your coverage. Here are the key benefits:
* These add-ons are subject to underwriting approval and your eligibility at the time of purchase or renewal
What Our Customers Have to Say about Us


Advantages of Cashless Medical Insurance
Cashless health insurance is a necessary coverage one should have in the time of an emergency. It has several advantages that can help you be stress-free and not worry about managing the large amount at the hospital. Here are a few advantages:
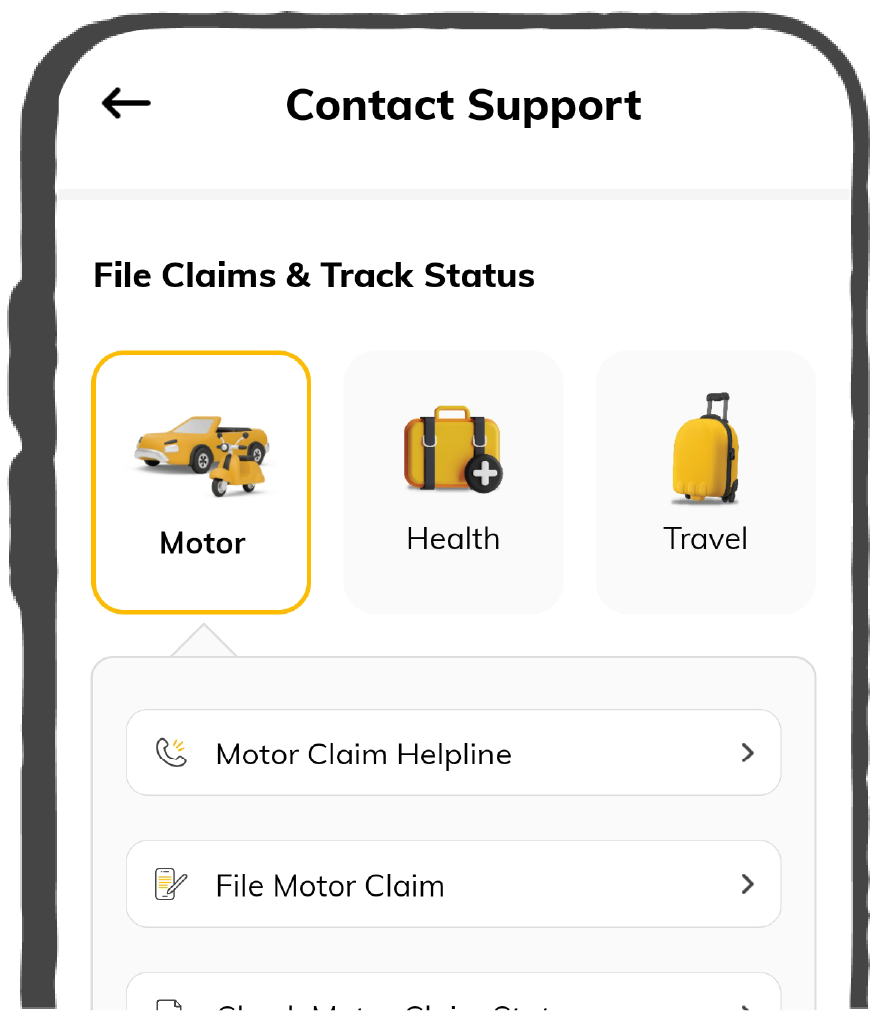
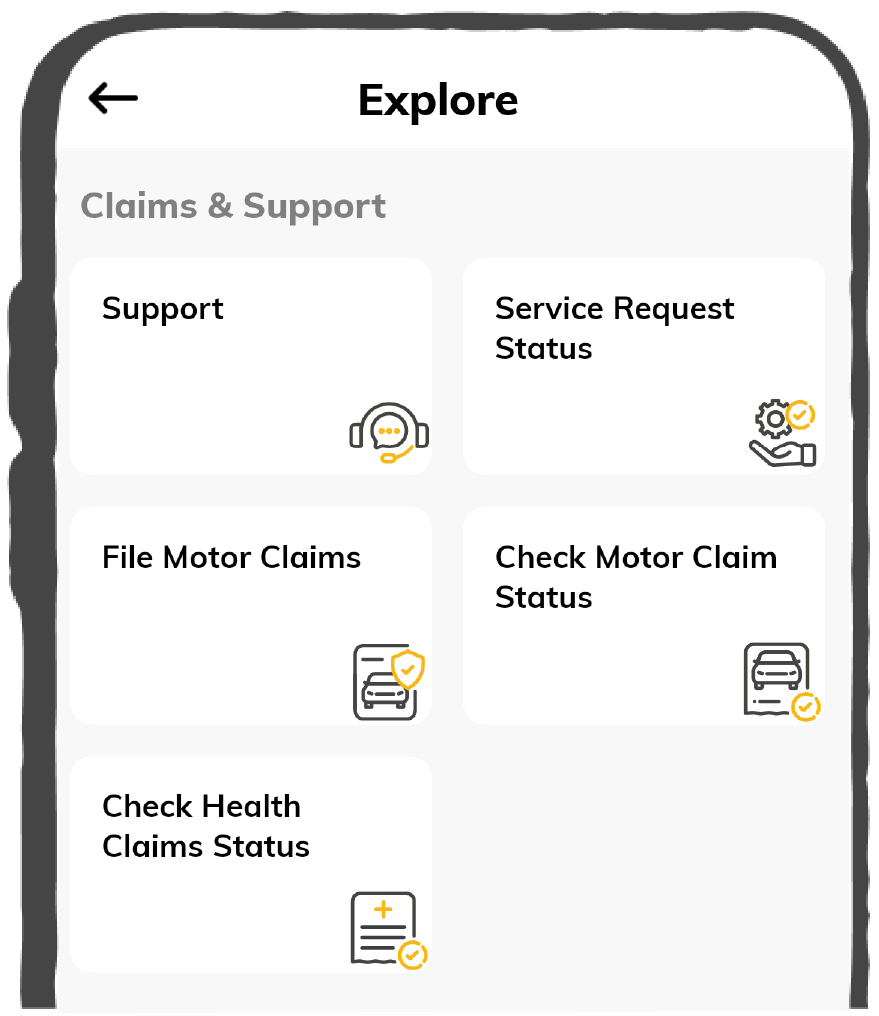
How to File a Cashless Claim with Digit?
Cashless health insurance ensures cashless anywhere, removing the inconvenience of having to pay cash at hospitals when necessary. Insurance companies bargain directly with hospitals in their network to pay for the insured person's medical care.
Here’s a glimpse into how it works and how you can make a cashless claim with your health insurance.
For Planned Hospitalisation
- When you need to make a health insurance claim, choose any one of our 9000+ network hospitals. These are the only hospitals where you’ll be able to claim for cashless treatment.
- Let us know at least 72 hours in advance if you’re going for a planned hospitalization in your preferred location hospital.
- When you visit one of our network hospitals, you must share your health e-card and ID proof with the hospital authority and obtain your pre-authorization form from the hospital.
- After your forms are all filled and signed, submit them and ensure the hospital shares these forms with the Third-Party Administrator (mediator between the hospital and your health insurer)
- Your request will be reviewed, and the insurance company will contact the hospital for pre-authorization. They will evaluate the coverage and medical necessity.
- The rest will be taken care of by your health insurer, i.e. us and the hospital!
For Emergency Situations
- You should start the cashless mediclaim facility within 24 hours of hospitalisation since you immediately require medical attention.
- At the network hospital, present your health insurance card, which will include your policy number, the name of your insurance provider, and the kind of policy you have.
- After completing the pre-authorization form, the insurance desk employee will accelerate the processing of your claim.
Documents Required for Cashless Hospitalisation Claim
You must have a few important documents when visiting a cashless hospital in India. With no upfront fees, this procedure makes your hospital stay easy and hassle-free. The documents include:
- Health E-Card (if any)
- Identity Proof: Driving Licence, Adhar Card, etc.
- Medical Documents: Doctor’s Prescription, Admission Form, etc.
- The hospital Pre-Authorization form filled
- Previous Medical History Reports
- Claim form downloaded from your insurance company website
- Any additional document required by your insurance company

Digit's Network Hospitals for Cashless Hospitals
Get Cashless Treatment at 9000+ Hospitals across India
Digit’s Health Insurance Claim Numbers for FY 2024-25
Digit Settled 9.16 Lakh Claims in FY 2024-25
The data below is for all the products as given in the table below:
What to Do If No Cashless Hospitals Are Nearby?
Although we hope that never occurs, you can file a reimbursement claim at any other hospital of your choosing in its place. Here's how to submit a claim for reimbursement:
- Notify us about your treatment within 48 hours after the date of hospitalisation
- Avail your treatment and settlement bills that you have done out of your pocket
- Submit and upload all the necessary documents on your company’s portal to get the reimbursement
- The insurance company (us) will verify all the documents and settle your claim after verifying.
Difference Between Cashless Claim and Reimbursement Claim
As mentioned above, there are two types of processes you can opt for during claims in health insurance. A cashless claim or a reimbursement claim. Here’s a quick table to help you understand the key differences between the two!
Top Reasons for Claim Rejection in a Cashless Medical Insurance
One excellent strategy to lessen the financial strain of medical bills in India is to use a cashless mediclaim policy coverage. Nonetheless, claims made under this policy may be denied for specific reasons.
Let's dissect it to make it easier to understand:
- Incomplete Waiting Period: There is a waiting period for specific conditions under every policy. You risk denying your claim if you file for a condition during this waiting time. Be sure you understand these waiting times for the specific treatment you are undergoing.
- Non-Disclosure of Information: Your claim may be denied if you hide any information regarding your health or any pertinent health information. Always fill out your policy application accurately and truthfully.
- False Information: The claim form may be rejected if it contains any false information. To prevent such issues, double-check all the information before filing the claim.
- Insufficient Documents: Failure to provide all required documentation is one of the primary causes of health claim rejection. Ensure that you provide the insurance company with all your medical documents, bills, and reports as requested.
- Pre-existing Conditions: Your claim may be denied if you haven't disclosed any pre-existing medical conditions when applying for insurance. Always provide your whole medical history to prevent your claim from being denied.
- Timeframe Crossed: If you fail to notify your insurance company of your hospital stay within the predetermined time window, your claim can be rejected.
Everywhere Cashless by GIC: Treatment Anytime, Anywhere!
The General Insurance Council (GIC) started the 'Cashless Everywhere' program to recreate the Indian health insurance market. By altering the traditional methods of filing health insurance claims, this program gives policyholders greater ease and versatility.
In the past, policyholders who wanted cashless treatment had to choose a network hospital. If they sought medical attention outside of these networks, they had to pay the full hospital fee before filing a reimbursement claim. However, the Cashless Everywhere Hospitals campaign lifted these limitations, enabling policyholders to get cashless care at any hospital, independent of network ties.
This is how Everywhere Cahsless works:
- Check if your hospital is on the list of everywhere cashless hospitals.
- Confirm with the hospital if they accept Anywhere Cashless.
- Inform your insurance company before the 48-hour planned hospitalization or within 24 hours of admission during medical emergencies like accidents.
- You have to fill out your claim form and ask your hospital to mail it to your insurance company.
In India, cashless health insurance has transformed the way people approach healthcare, offering peace of mind in times of medical need. With a simple e-card at a network hospital, policyholders can focus on their recovery. At the same time, the insurer takes care of the financial side—no waiting in long queues or arranging last-minute funds.